Hyperkalemia Intro
- Potassium is primarily an intracellular ion responsible for maintenance of the resting membrane potential for normal cell conduction.
- Serum measured potassium is typically between 3.5 and 5.0 mEq/L.
- Serum K greater than 5.0 mEq/L is generally considered the threshold for hyperkalemia.
- Potassium is mostly excreted via the kidneys, and the "classic" hyperkalemia patient is one who has missed several dialysis appointments complaining of paralysis or diffuse weakness.
Causes of HyperK
- Most commonly, renal failure.
- Transcelluar shift
- DKA
- Acidosis
- Other acid-base disturbances
- Medications
- RAAS or ACE inhibitors
Effects of HyperK
- Most drastically affect cardiac myocytes
- Conduction between myocytes is depressed, leading to slower conduction and widened QRS complexes, however, the rate of repolarization is increased.
- Leads to ominous “sine wave” pattern on ECG.
- Arrythmogenic
- May produce classic tall, “peaked” T waves on ECG.
- Conduction between myocytes is depressed, leading to slower conduction and widened QRS complexes, however, the rate of repolarization is increased.
- Stepwise ECG changes in hyperkalemia:
- 5.5-6.5 mEq/L - Peaked T Waves
- 6.5-7.5 mEq/L - P waves amplitude becomes smaller and PR intervals prolong
- 7.5-8.0 mEq/L - QRS becomes wide
- ECGs are not always sensitive for hyperkalemia. Patients may have a critical K with no changes on the ECG.
- Skeletal muscle tissue is also sensitive to hyperkalemia, and patients may present with weakness or paralysis as a result.
- Nondescript symptoms such as muscle cramps, diarrhea, vomiting, nausea, and focal paralysis may also be present - but are also not reliable findings.
Management
- Prioritized by a strategy of:
- Stabilization of cardiac cell membranes
- Shifting potassium back into the cells
- Eliminating potassium
- Calcium (Chloride or gluconate) administered to stabilize cell membranes
- Stabilizing effect is transient and relatively short lived
- Calcium Chloride contains roughly 3 times the amount of elemental calcium as compared to Ca gluconate, but is associated with severe complications if extravasation occurs.
- Effects (narrowing of QRS complex, return of more hemodynamic stability) occurs within minutes
- Calcium Chloride - generally, 1 gram is administered over 3 minutes.
- Calcium Gluconate - 1 gram over 2-3 minutes
- Repeat either q5min
- Albuterol / Beta 2 agonists
- These act on beta 2 receptors to assist in moving potassium back into the intracellular space
- Albuterol - 10-20mg (inhalation), with most effect noted in 30 minutes
- IV Insulin
- Drives K back into the cells (shift)
- Generally administered with dextrose unless the patient’s BGL is below 250mg/dL
- 10 units IVP followed by 25G dextrose
- Incidence of hypoglycemia is high, and this therapy should be administered cautiously
- Dialysis
- Treating reversible cause
- d/c RASS or ACE inhibiting medicaitions
- Volume administration
Show More
Rate
Join Podchaser to...
- Rate podcasts and episodes
- Follow podcasts and creators
- Create podcast and episode lists
- & much more
Episode Tags
Do you host or manage this podcast?
Claim and edit this page to your liking.
,Claim and edit this page to your liking.
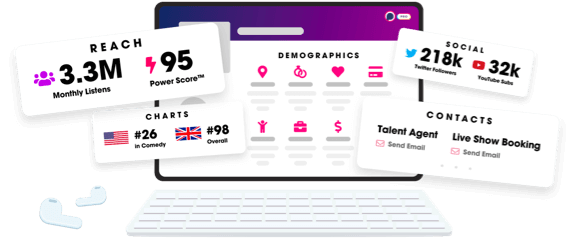
Unlock more with Podchaser Pro
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us
